Season 10 Case 22
History: Dementia, poor food intake


Answer:
CLICK HERE FOR ANSWER
Bilateral Mandibular Dislocation
If you came of Radiology age before the ubiquitous use of CT, you may have seen these; however these days, mandible series are quite rare (and perhaps deservedly so). My experience is that these days few Rads feel very comfortable with them.

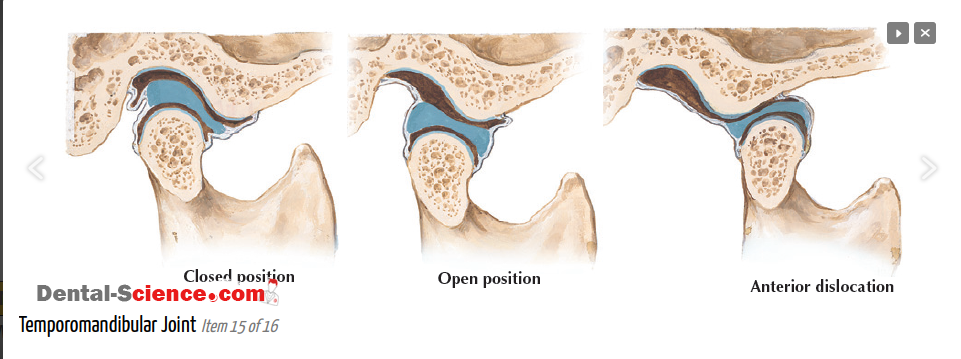
Anatomy
Here is a normal lateral view of the mandible/skull.
Green = temporomandibular fossa (aka glenoid fossa)
* anterior border is the articular tubercle (aka condylar eminence)
* posterior border is the tympanic portion of the temporal bone (behind which is the external auditory canal
Blue = mandibular condyle
Here you can see the mandibular condyle sitting in the glenoid fossa. There is a normal articular disc that sits between the cartilage of the mandibular condyle and the cartilage of the glenoid fossa which of course we just see as space on X-ray.
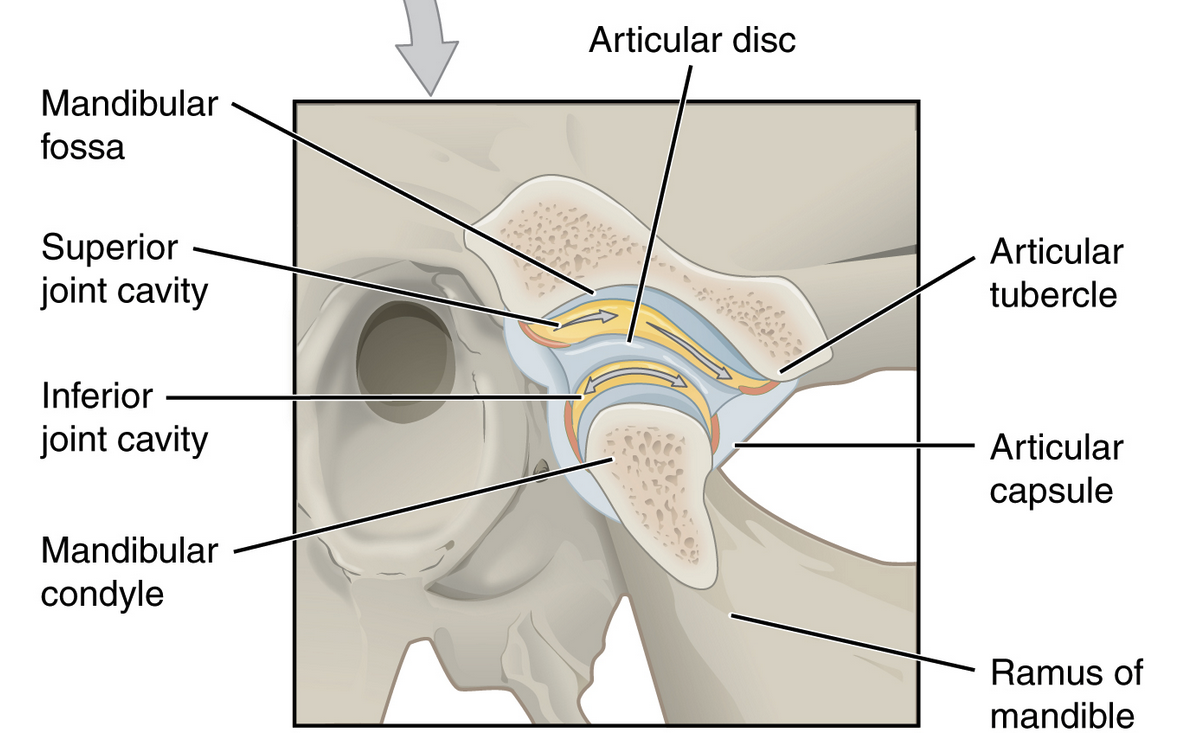
So if there is injury, or the capsule is loose from prior injury or degeneration, it is possible for the mandibular condyle to dislocate of the glenoid fossa, almost always anteriorly.
Posterior and superior (into the intercranial fossa) dislocations are rare.
Our Patient
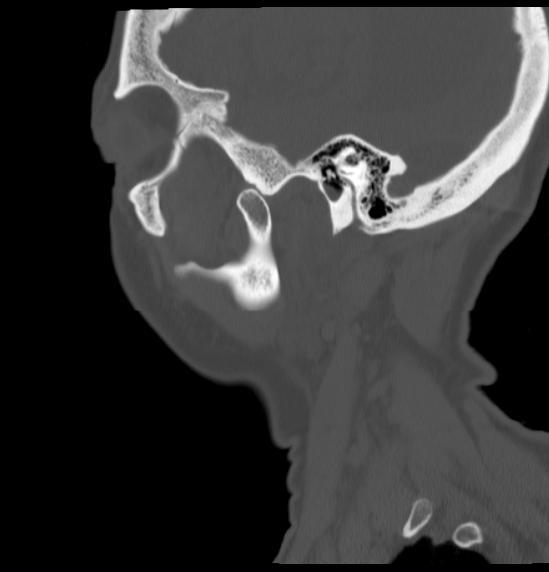
So lets look again at our patient.


Again, I've labeled the mandibular condyles and the temporomandibular fossa (aka glenoid fossa) for both sides.
Hopefully you can now see that BOTH the right and the left condyles are dislocated ANTERIOR to the fossa. For once symmetry is NOT your friend :(
But just in case you don't believe me:
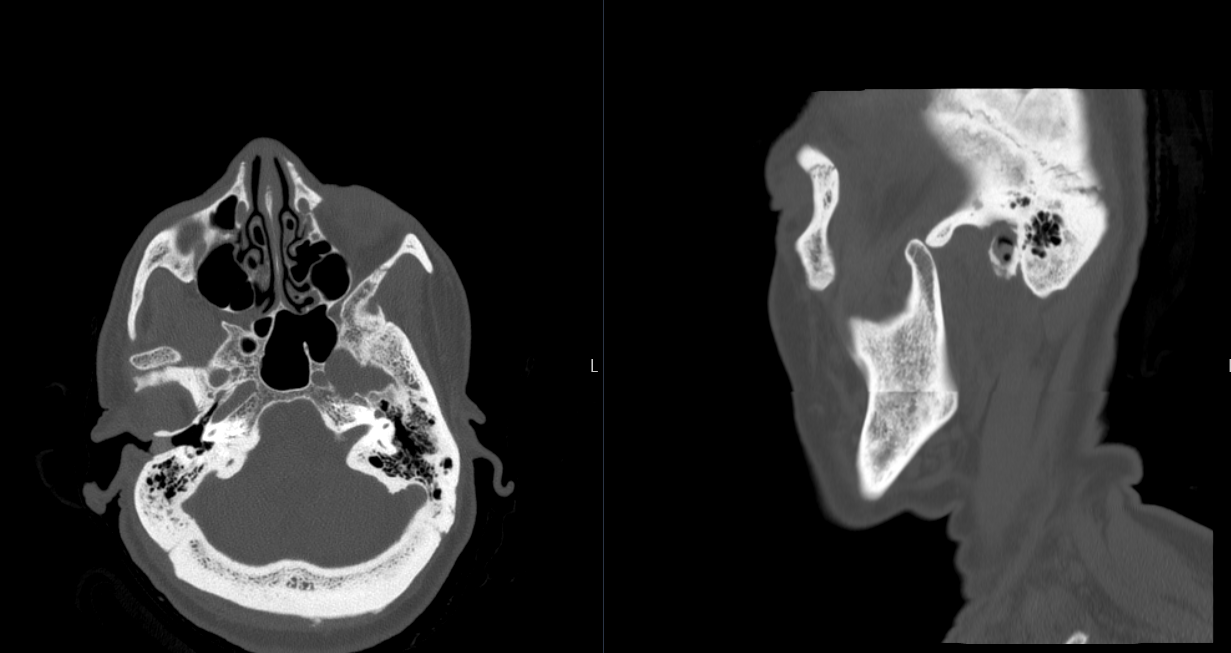
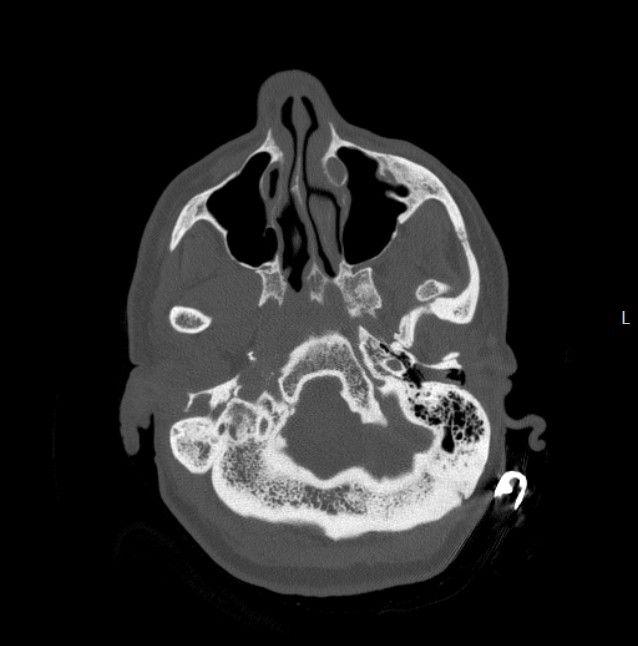
And for completeness, here is the axial CT labeled and centered on the left TMJ.
Our patient here had a history of prior dislocations so the CT was ordered for initial diagnosis and then the X-rays were ordered to confirm reduction. Unfortunately it was not reduced (which they suspected clinically).
They re-attempted reduction, which they believed to be successful, without additional imaging.
Movement
Movement of the TMJ is complex and can cause some confusion with dislocations. While MRI evaluation of the disc and motion is beyond the scope of this write-up, it is important to remember that the condyle normally moves forward with opening but it should not move beyond the lowest point of the articular tubercle. That is dislocation!
Why CT?
For all new dislocations (or concerns for dislocation), I would recommend utilizing CT for diagnosis, not just because of the limited experience with X-rays, but because you should always be on the lookout for a fracture (such as transcondylar, of the coronoid process, or even the glenoid fossa if there is significant trauma). These can be difficult to impossible (glenoid fx) to see on X-rays and of course management changes significantly.
*Plus, in the instance of trauma, you get to check out all the other bones of the face just in case.
Management
If you are interested in the management, here is a nice ER doc review: